Camera-Ready: Video Technology Improves Patient Care and Safety
At Houston Methodist, we are taking video technology to new heights with one focus in mind — our patients. Special cameras and sensors have been installed in patient rooms, ready to monitor patient activity and provide additional support for clinicians. It’s all part of a systemwide effort to improve patient care and satisfaction through video technologies.
What began with voice technology has broadly expanded and now includes video and smartboards to enhance the patient experience. The journey started in 2020, when we launched ambient listening. Similar to Amazon’s Alexa, we’re leveraging voice technology in patient rooms to enrich the patient experience and deliver real-time medication information.
“We’re finding more and more opportunities to improve the delivery and quality of patient care with ambient systems,” said Mark Vassallo, HM vice president of quality. “They can detect learned conditions with increased reliability, accountability, speed and accuracy. They also elevate the patient experience, with fewer interruptions, and enable our care teams to focus on patient needs only a bedside clinician can provide. It’s a win-win.”

Lights…Camera…Action – Dynamics of HM Smart Room Technology
Two initiatives are now underway in more than 150 patient rooms at HMH. They use special audio/visual systems, including wall-mounted cameras, sensors and smart video boards across from the patient’s bed.
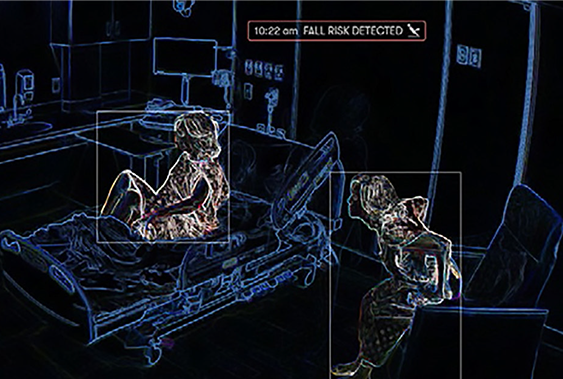
The first initiative is an in-room activity monitoring system. Special “M2” infrared sensors use learned or ambient intelligence to track specific actions in the patient’s room, like patient or care team movement in the room.
Having previously been programmed to “learn” the dynamics of patient rooms, like the proximity of a patient in the hospital bed or the location of various clinical equipment, the system can detect set activities and send critical alerts to clinicians.
For example, the first thing being monitored are patient fall risks. If the system detects that a patient is attempting to get out of bed, an alert is sent to the appropriate care team.
The second initiative is a new, SMART Board-enabled telenursing program. Connected to special “R2” cameras, a remote telenurse can be requested with the push of a button on the smartboard.
Much like a Zoom or FaceTime call, R2 cameras transmit live video of the patient to the telenurse. The patient can see and interact with the telenurse through their TV. The video is not recorded and is only activated at the request of a bedside clinician or after patients have acknowledged it is a good time to talk.
“We continue to utilize innovative technology at Houston Methodist to support our patient care and lighten the workload of bedside team members whenever possible. Ambient technology will play an increasingly important role as it supports patient safety in activities such as fall prevention,” said Gail Vozzella, HMH senior vice president and chief nursing executive. “With these digital devices, we are providing more data points to measure and improve patient care and staff satisfaction.”
Focusing on Patient Privacy, Care and Satisfaction
Protecting our patients’ privacy is always our number one concern. For that reason, the in-room sensors are only enabled on-demand and never store captured audio/visual data. At most, the infrared M2 sensors create a log of specific, identified events based on its observations. Interactions outside of those events are not recorded.
More notably for patients, the ambient monitoring system will provide an added layer of patient security. Like bed alarms and fall mats, the infrared “eye in the sky” alerts staff when patients are attempting to leave their beds. While the system does not need to be turned on for every patient, it can be activated for those already considered to be a fall risk. Patients can still use their call lights to notify the care team when help is needed.
The R2 camera can also connect a telenurse with the patient to provide education, answer questions or concerns and go through the discharge workflow, so patients can get home with thorough information.
“The virtual nurse was very helpful and nice. She answered my questions and really helped to keep me from getting too nervous about my treatment,” remarked an approving patient.

Supporting Staff in a Flash
For our care teams, these systems present opportunities to dedicate more focused attention to the clinical needs of our patients — the tasks that only they can perform. Bedside clinicians can more easily round on patients and administer medications while the new telenursing system manages new patient intake and some assessments.
“Telenursing and ambient monitoring systems are proven solutions that lead to greater satisfaction for patients and the nursing staff,” said Steve Klahn, HM virtual medicine – inpatient clinical director. “They provide opportunities to alleviate some of the demands we place on nurses, so they can focus on more pressing patient needs and enhance the overall level of care we provide. We’re optimistic about seeing positive results from the systems we are introducing.
Zooming in on the Future
The new M2 and R2 devices have been installed in several units at HMH, with plans to expand systemwide soon. With every click of the shutter, we’re finding new opportunities to ensure the best care and clinical outcomes for our patients.
There are opportunities to use the M2 infrared monitoring system to prevent pressure injuries, detect patient incontinence and ensure hand hygiene. By observing patients’ positioning and sending risk alerts, we can make sure turn schedules are followed and patients don’t remain idle too long, in one position. Using heat sensors, the system can also tell if a patient is suddenly wet or watch if staff uses hand sanitizer.
Our goal is that one day, the technology may also be integrated with Epic to automate documentation of key nursing tasks. This will free up our clinicians to spend more time caring for patients.
“The more we are able to integrate technology that can automate or simplify clinician workflows, the more likely we are to increase direct patient care, improve patient outcomes and decrease clinician burden,” said Lisa Stephenson, MSN, HM chief nursing informatics officer.
