The Rise of Remote Patient Monitoring Inside the Hospital
As we mentioned in the previous CIO Quarterly, remote patient monitoring (RPM) tools, such as BioButtons, are becoming an invaluable tool in acute care settings. This has been accelerated in recent years by the COVID-19 pandemic, offering continuous surveillance and early detection of changes in patient conditions.
Below are insights published in Houston Methodist’s digital innovation newsletter on LinkedIn by Gail M. Vozzella, SVP, CNE, and Sarah N. Pletcher, MD, MHCDS, that cover our vital signs monitoring program, our activities to-date, how it’s beneficial to our patients and what’s on the horizon.
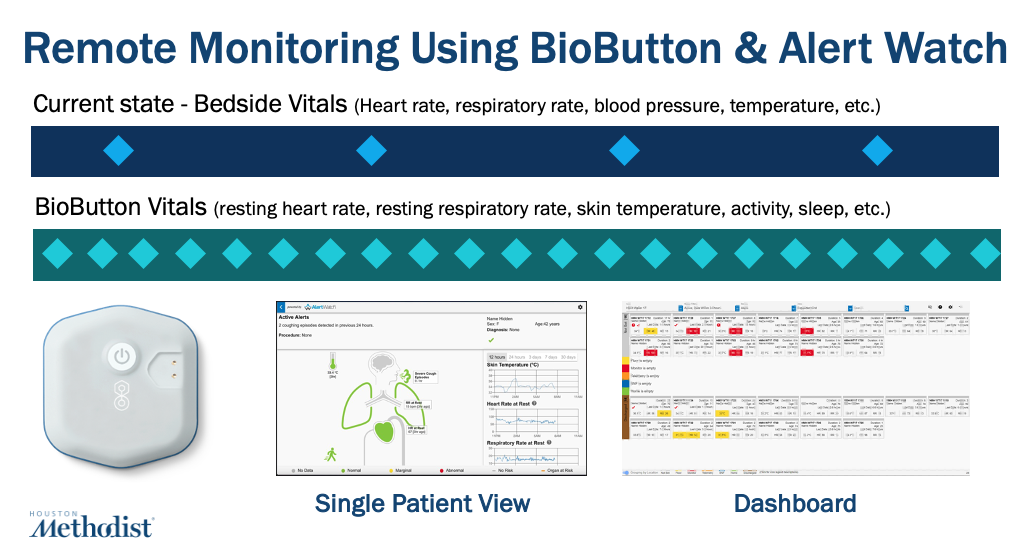
While continuous vital sign monitoring by virtual care teams was previously limited to and studied in settings like the intensive care unit (ICU), the newest generation of multiparameter wearable medical devices can be used on all hospital patients. These high-tech tools provide our health care teams with continuous data on vital signs and other clinical data points, overseen by a central virtual monitoring team who utilize monitoring dashboard software that applies sophisticated analytics and algorithms to improve patient safety by facilitating earlier interventions.
Houston Methodist launched a vitals signs monitoring program, using the BioIntelliSense, Inc BioButton across acute care units beginning in April 2023, starting at our acute care main hospital in the Texas Medical Center. The project has since been taken to scale across 2,600 beds in all eight Houston Methodist hospitals.

How It Works
- The small battery operated BioButton is adhered to the patient’s chest upon hospital admission.
- The device measures heart rate, respiratory rate and skin temperature up to minute-level frequency.
- A dynamic monitoring dashboard alerts when a patient’s trending data triggers algorithms.
- Workflows have been developed for the virtual operations team to respond to alerts, assess and investigate, confirm and discuss patient status with the bedside nursing team, and escalate to provider teams where appropriate for immediate assessment and intervention.
Despite the importance of respiratory rate as an early indicator of clinical deterioration, an integrative literature review by Palmer et al. (2023) found that clinical staff are not correctly assessing respiratory rate due to errors via estimation, count and multiply techniques, and value bias. This results in nearly all patients documented as breathing between 12-20 times per minute. Utilizing RPM technology that objectively measures chest wall motion of breathing, we now see a range of patient respiratory rates, receive alerts for patients outside the parameters, and can intervene and assess patients more quickly. RPM has led to objective reductions in patient severity at the time of entry to the ICU for patients who have required immediate interventions such as rapid response.
Benefits and Beyond
Another benefit of central monitoring using BioButtons is that we have safely reduced the frequency of bedside patient vital sign collection by a medical assistant from every four hours to every eight hours. The extra time freed up for bedside teams allows them to follow up on call lights more easily or provide personal care tasks to patients. Vital sign frequency reduction is based on calculating 5 minutes per patient 3 times daily over 250,000 patient days which amounts to over 62,000 person-dedicated hours that can be given to other patients who need hands-on care. Reduced vital sign checks also gives patients uninterrupted hours overnight, hopefully allowing patients more time for rest and sleep, which is essential to recovery and delirium prevention, especially in the older adult population.

As evidenced by our initial success using the BioButton, RPM will continue to be an important tool for inpatient use, especially considering the high acuity of patients and the significant reduction in resource utilization. Our next step is to test the BioButton in the home setting, equipping patients with the device as part of the hospital discharge process, which will allow our clinicians to continue monitoring patients during their recovery period after they leave the hospital.
References:
Palmer, J. H., James, S., Wadsworth, D., Gordon, C. J., & Craft, J. (2023). How registered nurses are measuring respiratory rates in adult acute care health settings: An integrative review. Journal of clinical nursing, 32(15-16), 4515–4527. https://doi.org/10.1111/jocn.16522
