Leveraging Digital Technology to Ensure an Unparalleled Experience
[Note: This article was written by Ashleigh Kamencik-Wright, program director, and Courtenay Bruce, associate chief experience officer, and was originally published earlier this year in Roberta Schwartz’s DIOP Newsletter on LinkedIn.]
We have all been a patient or a caregiver. Navigating the health care environment can be a complex and confusing experience. One of the most difficult tasks as a patient or caregiver is trying to remember what to do, what not to do, and what signs or symptoms should be considered alarming. Studies have shown that 40-80% of communicated medical information to patients and caregivers is forgotten immediately. Additionally, the more information presented, the less likely the information will be recalled correctly. Indeed, almost half of the information communicated will be remembered incorrectly.
As health care professionals, we are cognizant that preparation, education and communication are critical for every patient’s successful recovery. At the same time, we all know that patients and caregivers are overwhelmed by lengthy and sometimes complex instructions, which can lead to non-adherence, missed appointments, canceled surgeries, longer lengths of stay, emergency department revisits or readmissions.
To mitigate these issues and fully prepare patients and caregivers, we at Houston Methodist utilize digital technology to bridge communication and education gaps. We developed a library of digital inpatient and outpatient care pathways that allow us to clinically monitor our patients, receive real-time feedback, and communicate at just the right moment.

Outpatient Care Pathways
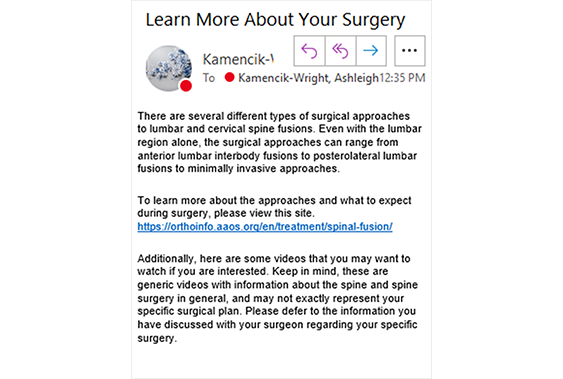
Patients receive educational content, reminders and monitoring questions by email and text — based on their preference — at predetermined intervals. Information and instructions are delivered at the most relevant time in small bite-sized chunks, prompting patients to adhere to care instructions. Messages are sent between 15 and 30 days before hospital care (about one message sent every couple of days) and continue for 30 to 60 days afterward, with a message every few days. Text messages contain information that should be addressed timely — such as a reminder to take medications or not to eat after midnight. Example messages include how to prepare for a procedure, what to expect at the hospital, care at home, lifestyle changes, and when to call their physician’s office or go to the emergency department if they are experiencing concerning symptoms. On the day before surgery, patients might be reminded: “Now is time to take your bowel prep! Here are the instructions on how to do so…” Email messages answer frequently asked questions of past patients that have been identified by the care team through our experience with continued use of the pathways.

Teams of Houston Methodist physicians, nurses and other health care professionals wrote and developed each message and pathway, and many of them created videos to supplement the educational messages. Patients can also appoint a caregiver, the individual that will be helping them to recover at home, to receive the same educational content as the patient and they will both learn about the patient’s condition, care at home, and what to expect. Additionally, we ask patients and caregivers questions about current symptoms and concerns — functioning as an effective clinical monitoring tool during critical times by routing clinical alerts to the patient’s clinicians. This routing system allows physicians to intervene as early as possible to mitigate potential complications.
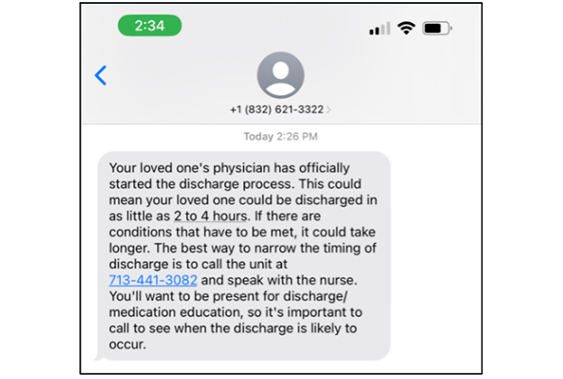
Inpatient Care Pathways
When patients are admitted, they are asked if they would like anyone to receive text message updates about their progress — friends or family members. Those contacts are entered into Epic, our electronic medical record (EMR), as a visit contact. All clinical staff with access to flowsheets in Epic can send text message health care updates to the contacts that the patient has identified. Additionally, we send the contacts information when the patient has been transferred to another unit, the expected date of discharge, explanation of the discharge process, information on care coordination rounds, the room number, and the room phone number.
Every three days, we ask the patient’s visit contacts to reflect on their experience with the communication and to provide us with feedback. If they indicate that they are dissatisfied, we ask them to elaborate, utilizing a free text field. A notification is sent out to the unit leadership every morning and evening with their dissatisfaction alerts from family members. This gives the unit leadership the opportunity to address concerns and conduct service recovery real-time before the patient is discharged.
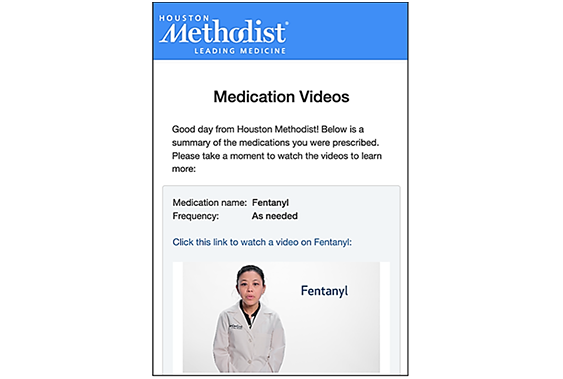
Patients also receive information via text message on their medications while they are in the hospital and after they are discharged home. When the nurse scans the medication in Epic, a text message is sent out to the patient that contains a short video. This video addresses what the medication is prescribed for, what are the possible side effects, and explains which symptoms are concerning. The patient is asked if they have any additional questions for a pharmacist. If they indicate that they do have questions, an alert is sent to the floor pharmacist so they can round on the patient to answer their questions. Once the patient is discharged, they will receive one final text message of medication videos that corresponds to their discharge medications.
These inpatient messages help to strengthen patient experience by keeping the patient and the patient’s contacts informed through a convenient mechanism. It also decreases phone calls by keeping the contacts proactively informed. We have received thousands of family comments from patient caregivers stating that they ‘felt like they could go home and shower’, or that ‘they didn’t feel like they needed to campout in the patient’s room’, or ‘they can’t use the phone at work, so text messaging is ideal’. These comments suggest that the texts provide emotional and cognitive relief, allow for richer understanding, and help family members navigate their everyday life and responsibilities while the patient is admitted.
Summary of Results:
- $1.3 million in savings per service line.
- 14% increase in HCHAPS satisfaction.
- Less than 1% opt out rate.
- 55% reduction in readmissions.
- Surgery cancellations below 3%.
- 30% reduction in office phone calls.