Cultivating a Clinical Communications Culture
Compassionate communications with patients and between clinicians are essential parts of Houston Methodist’s pathway to unparalleled, impacting patient care and safety. While Houston Methodist is fortunate to have several resources available to foster good communications between providers, nurses and medical staff, it can be challenging determining which tools to use. To cultivate and improve communication systemwide, an initiative is underway led by Dr. Jordan Dale, HM chief medical information officer and Lisa Stephenson, HM chief nursing informatics officer.
“During a patient emergency, our nurses need to reach the right providers, using the most relevant tools. At the same time, our providers need to make sure their on-call schedules are complete and current, so the correct contact is reached, and they aren’t disturbed unnecessarily,” explained Stephenson. “We have good communications tools, but they’re only effective when we’re using them properly.”
Emphasizing the when, what and how
When patient care is on the line, providers and clinicians must be able to reach each other quickly and efficiently. Every minute spent messaging the wrong provider or searching for the correct contact details is frustrating and may delay patient care.
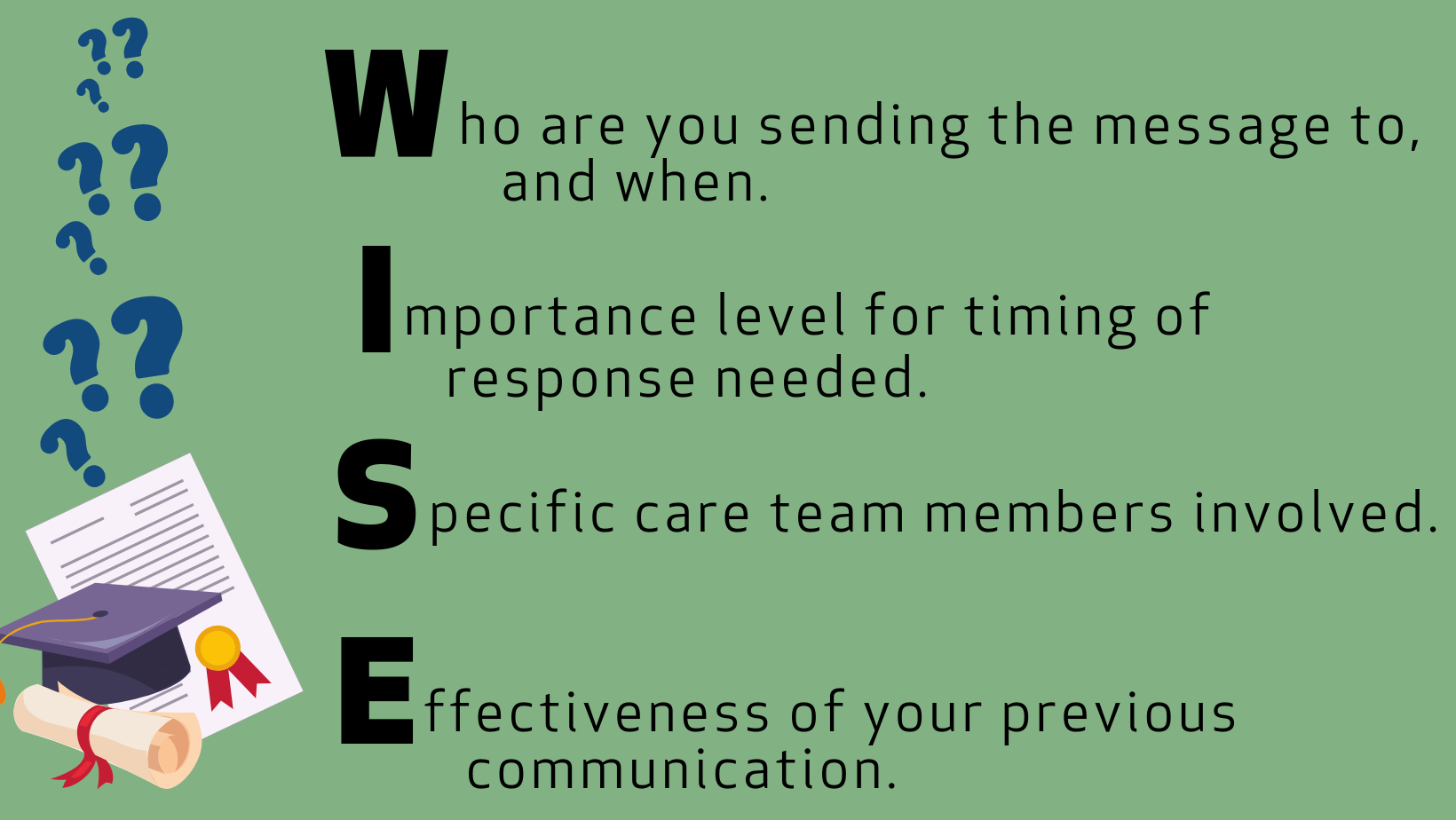
The culture of communications at HM focuses on four essential factors: understanding the urgency of the situation, respecting the timing of messages, identifying the correct recipients and determining if and when the message needs to be escalated. An easy way to think about this is to remember the acronym WISE (see visual).
New tools to help you
New tools, like QGenda, our systemwide on-call platform, or On-Call Finder, make it easier to find providers’ preferred contact methods and details. Both indicate when a call or page is appropriate or if a message through Secure Chat will suffice. QGenda works within Epic to serve as a single source to help you identify who’s on-call. On-Call Finder helps you find on-call providers’ contact details. The first clinical groups at HMCCH, HMCL, HMH and HMW began transitioning to QGenda on July 24.
“We need to leverage the same technology that moved us apart to bring us back together,” said Dr. Peter Nguyen, FACP, FASN, HM associate chief medical information officer and HMH medical staff president. “Oftentimes, we don’t know who’s on call, when they’re on call and more importantly, how to call. Some simple things we can do to help facilitate communication include: put a preferred contact method in your note; outline contingency planning, like weekend or holiday coverage; and reach out to the care team if key changes occur.”
Of course, the on-call schedules and contact details must be maintained and kept up to date. Each provider’s notes and documentation should be clear and current for hospitalists and other clinicians to understand and follow your plan of care, as well as react to changes in patients’ vitals.
Additionally, approximately 2,500 new iPhones will replace shared mobile devices (currently TC52 phones) through early 2024.These phones will continue using Rover for Epic integrations, with push notifications from Secure Chat to improve awareness of direct messaging. OAs can also use the new phones to view on-call schedules, phone directories and patient care teams.
Plans are in development to route bedside alerts to the correct clinicians and staff, instead of pinging everyone or just the unit administrative assistant (UAA).
Your next steps
This initiative is just one step, but we also need your support. “It’s essential that everyone understands and respects the expectations set around communicating with other team members in the most effective and efficient manner,” added Dr. Dale. “In some cases, we’re introducing new ways to communicate, and we must be open to these changes. Ultimately, this will help us work more collaboratively together.”
Here are ways you can help:
- First and foremost, assign yourself to your patients’ care teams. In doing so, you ensure the correct care team members receive patient messages and alerts. When you’re no longer on the treatment team, removing yourself will also stop unnecessary messaging.
- To reduce unnecessary, late-night messaging, you should refrain from using Secure Chat for communication outside of your unit between 11 p.m. and 7 a.m. This allows for more focused messaging, when most care teams are available.
- If a provider, resident or OA is needed, use the on-call schedule/directory or follow the instructions from the attending physician or page operator to contact the hospitalist or resident. Review our clinical communication escalation plan here.
As we strive to be unparalleled, that must include excellence in our clinical communications. With new tools and a renewed culture, we’re taking the right steps for better communication with each other that should positively impact the care we provide to our patients.

