A New Era of Connectivity and Care: Transforming Clinical Communication at Houston Methodist
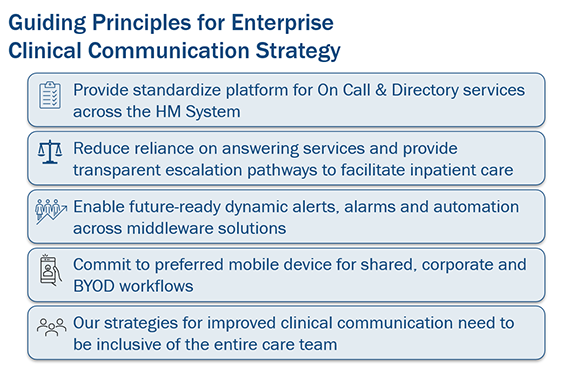
Over the past two years, Houston Methodist has been modernizing the platform for how care teams connect, coordinate and respond, laying the groundwork for a more agile and responsive clinical environment. This transformation is focused on exceptional, patient-centered care and collaboration between all care team members and is guided by five core principles.
From systemwide deployment of mobile technology, to smarter alarm routing and streamlined emergency activations, these principles have shaped every innovation.
“Our clinical communication transformation is about more than technology,” said Dr. Jordan Dale, HM chief medical information officer and chief health AI officer. “It’s about creating a connected ecosystem that empowers every member of the care team. By following our guiding principles — standardization, transparency, automation, mobility and inclusivity — we’re building a foundation for faster decisions, safer care and better patient outcomes.”
Empowering Clinicians with Mobile Technology
One of the most visible changes is the broad deployment of iPhones in inpatient clinical areas. More than 3,600 shared iPhones have been distributed to nurses, patient care assistants (PCAs), therapists, technicians and other frontline roles. These devices are now central to daily operations, enabling secure communication, real-time access to patient data and faster response times.
On these phones are two key apps: Vocera Edge and Epic Rover. Vocera Edge supports secure voice communication, while Epic Rover utilizes Secure Chat for text-based communication. With Rover, clinicians also have mobile access to patient charts, medication administration and documentation.
“Mobile tools are no longer optional, they’re essential,” said Gail Vozzella, senior vice president and chief nurse executive. “We’re equipping our clinicians with the technology they need to make decisions quickly and stay connected, no matter where they are in the hospital.”
Physicians and advanced practice providers (APPs) are also encouraged to bring their own devices (BYOD) and install Epic Haiku/Canto and Vocera Edge, now accessible without installing InTune Company Portal. This flexibility supports personalized workflows while maintaining secure access to HM’s network.
Smarter Scheduling and Role-Based Communication
To standardize operations, we’ve adopted QGenda which integrates into Epic On Call Finder to allow staff to easily identify who’s on call. “We’re reducing friction in communication,” said Dr. Dale. “By focusing on roles and responsibilities, we’re helping teams collaborate more effectively and spend more time with patients.”
Integrated Alerts and Alarms: Smarter Routing, Faster Response
The next step in our journey is our alerts and alarms integration, a major advancement that ensures patient requests and emergency alerts are sent to the right caregivers via their shared clinical iPhones.
Here’s how it works:
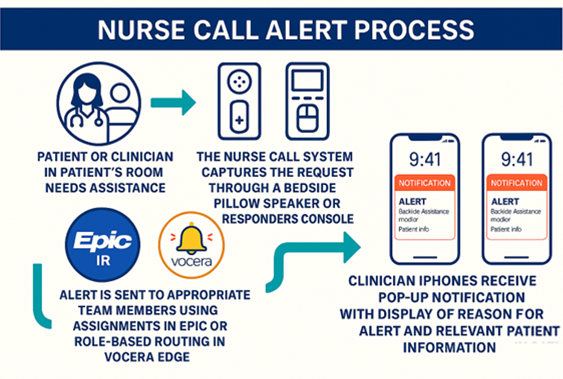
Example workflows include:
- Patient calls for assistance: Alert goes to the PCA assigned to the patient; if unanswered, it escalates to the RN.
- Staff Assist requests: Notifies PCA, RN, Charge Nurse and tech roles assigned to the patient.
- Emergency situations (CERT or Code Blue): Alerts are routed to all roles assigned to the patient as a critical alert.
These workflows are currently being optimized at HMCY, HMW and HMWB, where staff and patient feedback has been overwhelmingly positive. Teams report more efficient responses to patient needs and improved coordination during emergencies. Plans are underway to expand nurse call integration to additional hospitals, with more details coming soon.
Emergency Team Activation: Faster, Smarter Response
In high-stakes situations, every second counts. HM is advancing our emergency response capabilities by transitioning critical care team activations — including STEMI, stroke, telestroke and emergent large vessel occlusion (ELVO) — from PerfectServe to Epic.
This new process provides a more seamless, reliable and integrated solution for clinical communication and team coordination, while streamlining operations and improving response times across key clinical scenarios. “This is about saving lives,” said Dr. Dale. “We’ve built a system that supports fast, coordinated action, because in emergencies, communication is everything.”
By embedding notifications and assignments directly within Epic, we’ve eliminated the need to toggle between platforms and minimized errors due to fragmented systems. When a critical care order is placed, Epic will send alerts to response team members through Epic Rover or Haiku. Messages will include relevant details for the activation and information from patient charts, as well as the ability to communicate with each other through Epic’s Secure Chat.
What’s Ahead
“With these efforts we’re not just adopting new tools, we’re transforming how we work,” said Vozzella. “This is a cultural shift, and it’s happening because our teams are embracing change and putting patients first.”
Future enhancements for the clinical communication transformation will focus on:
- Expanding mobile access to more roles and departments.
- Enhancing app functionality for documentation, messaging and alerts.
- Improving cross-campus coordination for systemwide care teams.
