Medical Imaging Technology: You’ve Come a Long Way
Medical imaging technology has come a long way. Long ago, the idea of looking into the human body was just that — an idea. After the first X-ray was discovered, many other technologies were developed, like CT scans, ultrasounds, MRIs and nuclear medicine, giving clinicians access to valuable patient diagnostic information and imaging-guided therapeutics. Now, new innovations are improving patient care and satisfaction and helping providers make more informed care decisions — leading to better outcomes.
Imaging on the move: Portable technology means better bedside patient care
In the past, patients had to be moved to get their imaging. Yet, transferring patients to another area that houses that equipment isn’t always ideal and can pose risks for our patients. With the latest portable imaging technologies, digital X-ray systems, point-of-care ultrasounds and bedside CTs and MRIs, clinicians can now gather patients’ images and provide necessary therapies — at the patient’s bedside — reducing the need to physically transfer patients.
“Portable imaging used at the patient’s bedside accelerates turnaround times from order to diagnosis,” said Khalil Salman, MD CIIP, vice chair of informatics/AI and HM director of imaging information & AI. “This is a value to both providers and patients, but portable imaging is particularly valuable when moving patients may put them at risk, for example, ICU patients or patients with attached devices, such as tubes or lines. Imaging and imaging-guided procedures at the bedside can help mitigate that risk.”
Artificial intelligence: Driving more informed patient-care decisions
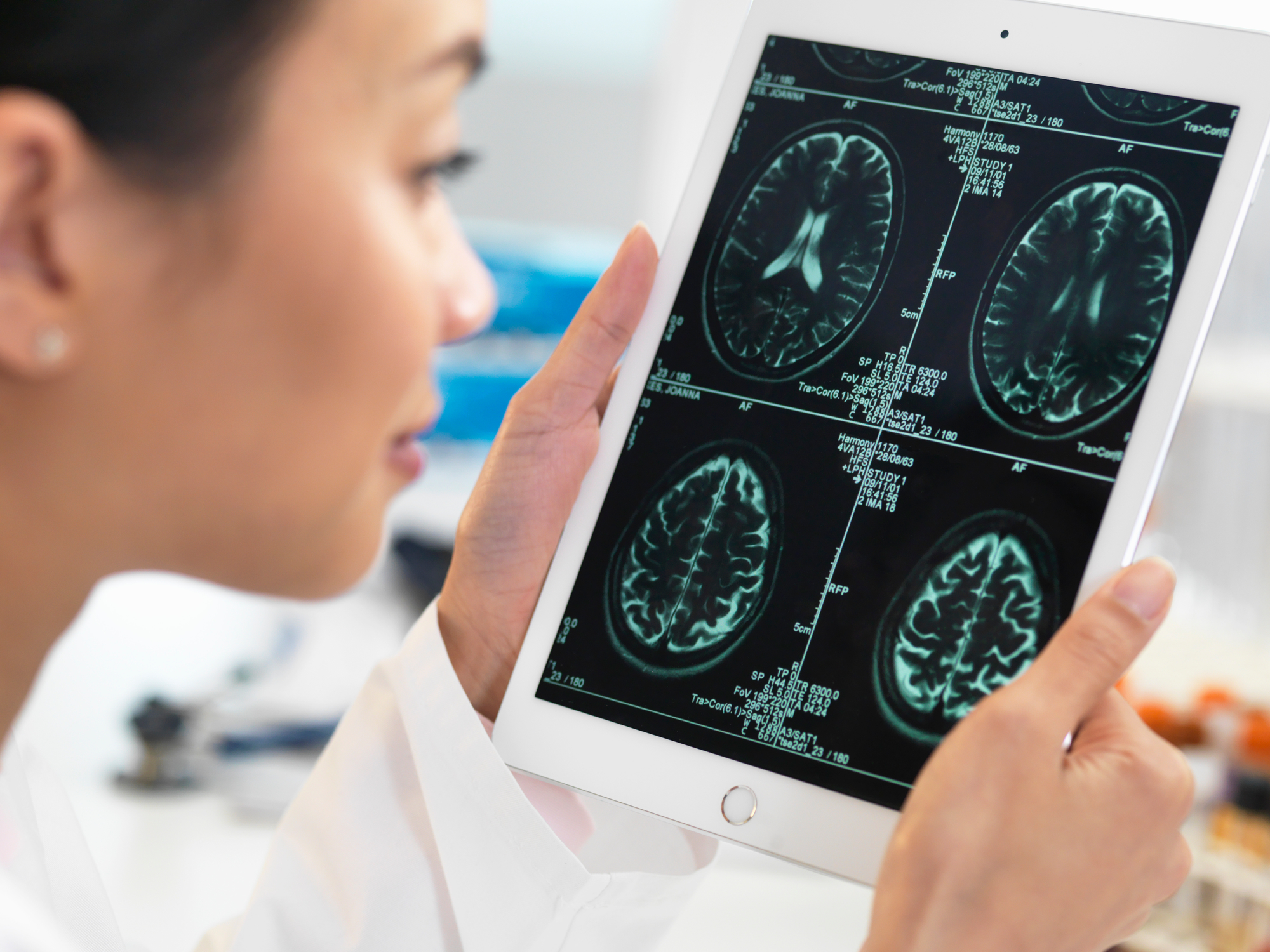
While portable imaging helps providers obtain images and administer image-guided therapies at the patient’s bedside, artificial intelligence (AI) in medical imaging is transforming image quality, reducing errors and helping to detect any abnormalities that warrant urgent attention and care.
“AI algorithms can be trained to automatically identify and classify abnormalities in medical images, such as detecting tumors, aneurysms or other irregularities in CT or MRI scans,” said Salman. “This can help radiologists identify and diagnose diseases more quickly and accurately and can reduce the number of false negatives (cases where an abnormality is present but not detected).”
It can also be used to assist with image analysis tasks, such as segmentation (identifying and outlining specific structures within an image) and registration (aligning images from different modalities or taken at different times). This helps radiologists to more easily compare and analyze images and make more informed patient care decisions.
“AI gives providers access to large amounts of imaging and clinical data, which can help with treatment decisions,” said Salman. “AI algorithms can be used to analyze large datasets of imaging studies to identify patterns and associations that might not be apparent to radiologists working with smaller sets of data,” said Salman. “This gives radiologists valuable insight that can help improve patient outcomes. AI has already had a role in accelerating diagnosis and treatment of our acute care patients. An excellent example is the Stroke Team’s implementation of Rapid-AI for on-site, immediate classification of CT scans obtained in the Emergency Department. Stroke patients who will benefit from a Neuro-Interventional procedure to remove a blood clot from the brain can have reduction of time to the procedure using AI, which can preserve brain function and improve outcomes.”
Follow-up evaluations and the accuracy of diagnoses are also improved with AI.

“Incidental findings often require additional evaluations or follow-up imaging studies, and AI can help radiologists prioritize follow-up evaluations based on the significance of these findings,” said Salman. “It’s also enhancing diagnosis accuracy. AI algorithms can be used to assist radiologists in their interpretation of images by providing additional information and context, which can enhance the accuracy of diagnoses and improve patient outcomes.”
“AI is helping to reduce radiologists’ workloads by automating routine tasks, such as image marking and report generation,” said Salman. “This allows them to focus on more complex and challenging tasks and can reduce the time required to complete an imaging study, driving better patient care.”
On the horizon: The future of AI at HM
Future AI implementations at HM will help automate or optimize certain tasks, allowing providers to focus more on providing personalized, high-quality care to their patients.
“We’re seeing AI integrating into all aspects of medical imaging, and we expect significant impact in everything from improved scheduling, patient communications, reduced scan times and improved integration with our other informatics systems used for communicating with our patients’ care teams,” said Salman.
“From the clinical side, Houston Methodist continues to seek new partnerships with vendors that allow our systems to incorporate AI,” said Salman. “Instead of implementing one AI solution at a time, we’re looking at systems that work like the Apple App store, that would allow us to evaluate and compare different AI algorithms prior to purchasing them. These systems would also allow us to build and test our own research algorithms, following our HMRI guidelines for responsible research.”
“While there are so many benefits to using AI, providers are still in the driver’s seat when making decisions,” said Salman. “Radiologists are still needed and required to interpret images and validate them, and as beneficial as AI can be, it can’t replace a radiologist’s expertise in providing the best care for our patients.”

